Healthcare data is everywhere—but trapped. Locked inside different systems, stuck in silos, and often impossible to access when it’s needed most. When doctors, labs, pharmacies, and apps can instantly share patient information without barriers, care becomes faster, safer, and more efficient. That’s the power of healthcare APIs. These behind-the-scenes digital connectors are revolutionizing how health data moves, enabling true interoperability and transforming patient care from fragmented to frictionless. In this blog, we’ll explore how APIs are changing the game. Let’s dive in.
Key Benefits of Healthcare APIs for Interoperability
Healthcare APIs are catalysts for change in the healthcare data landscape. Their ability to connect disparate systems creates multiple benefits that enhance clinical care, operational efficiency, and patient experience.
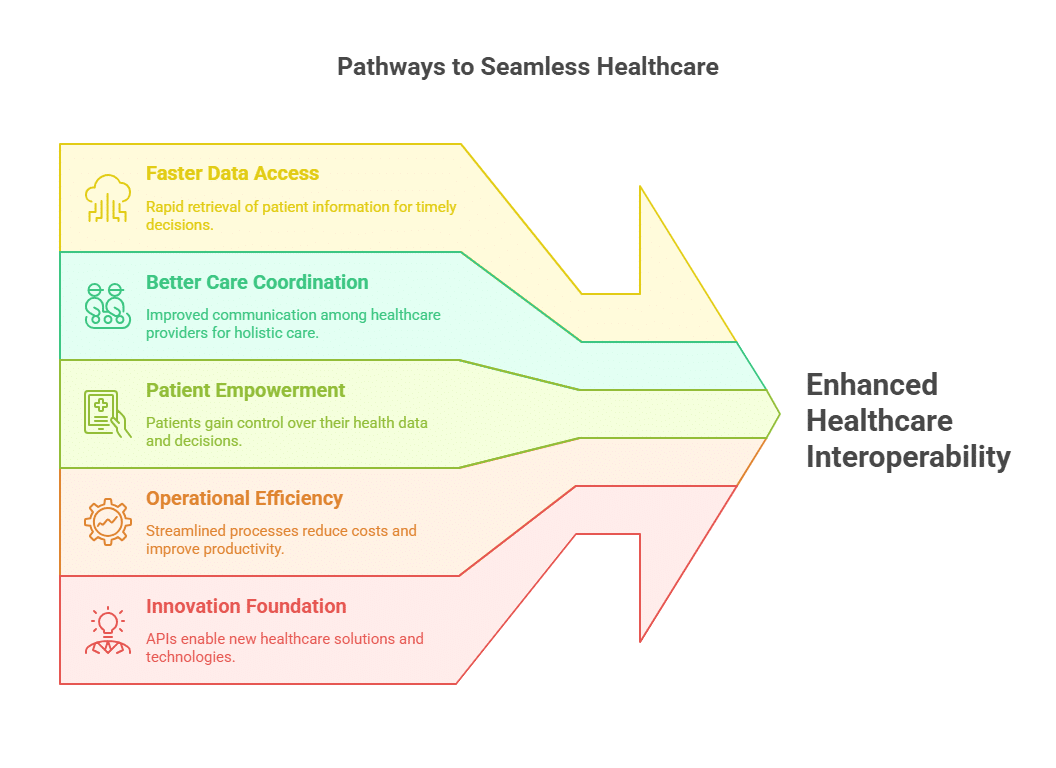
1. Faster and More Accurate Data Access
Timely access to accurate patient data is critical for quality care. APIs allow healthcare providers to retrieve comprehensive patient information—such as allergies, medication histories, lab results, and imaging reports—in real-time, regardless of where the data is stored. This immediate availability aids clinical decision-making and reduces the risk of medical errors.
For example, in emergency situations, having instant access to a patient’s full medical history can be lifesaving. According to a study by the Office of the National Coordinator for Health Information Technology (ONC), providers using API-enabled systems access external health data significantly faster than those relying on traditional data exchange methods.
2. Enhanced Care Coordination
Patients often interact with multiple providers, specialists, and pharmacies. APIs ensure that all members of a care team have consistent, up-to-date patient data. This unified view helps avoid duplicate tests, conflicting treatments, miscommunication, improving care coordination, and patient safety.
The Veterans Health Administration’s deployment of FHIR-based APIs across its nationwide network has helped reduce hospital readmissions by improving data sharing between facilities and care teams.
3. Empowered Patient Engagement
APIs also empower patients by granting them secure access to their own health data through apps and portals. This transparency encourages patients to actively participate in managing their health, resulting in better adherence to treatment plans and improved outcomes.
Apple Health Records is a prominent example, leveraging FHIR APIs to aggregate data from multiple providers into one accessible mobile interface, putting health information directly into patients’ hands.
4. Increased Operational Efficiency and Cost Savings
Healthcare organizations benefit operationally from API-driven interoperability by automating data exchange processes. This reduces manual data entry, minimizes errors, and speeds up administrative workflows.
The Mayo Clinic reported a 30% reduction in clinician time spent retrieving patient data after integrating APIs, freeing up valuable time for direct patient care and reducing costs associated with data handling errors.
5. Foundation for Innovation
APIs provide the infrastructure for next-generation healthcare solutions, including telemedicine, remote patient monitoring, and artificial intelligence-driven diagnostics. By providing standardized access to patient data, APIs enable these technologies to operate cohesively within healthcare ecosystems.
Wearable health devices, for example, continuously collect vital signs and transmit data via APIs to clinical platforms, facilitating proactive care and early intervention.
How APIs Enable Interoperability
Understanding how healthcare APIs work is essential to appreciating their role in driving interoperability. At their core, APIs are sets of protocols that define how software applications communicate. In healthcare, APIs facilitate secure, structured data exchange between heterogeneous systems.
Standardized Data Formats: The Importance of FHIR and Other Standards
One of the biggest hurdles in healthcare interoperability is the diversity of data formats and coding systems used across platforms. APIs solve this by adhering to widely accepted data standards, ensuring that data exchange is consistently structured and meaningful.
The most significant standard today is FHIR (Fast Healthcare Interoperability Resources), developed by HL7 International. Unlike older standards, FHIR is designed with modern web technologies in mind, utilizing RESTful APIs, JSON, and XML. It breaks down healthcare data into modular “resources” such as Patient, Observation, Medication, and Appointment, each with a clearly defined structure.
By using FHIR-compliant APIs, systems can exchange complex healthcare data accurately. For instance, a hospital EHR can share patient allergy information with a pharmacy system, enabling safe medication dispensing without ambiguity or misinterpretation.
Other standards also play important roles. DICOM handles medical imaging data, ensuring seamless transfer of X-rays, MRIs, and CT scans, while HL7v2 continues to support many existing messaging workflows in healthcare.
Secure Data Transfer: Safeguarding Sensitive Information
Healthcare APIs embed strong security protocols to protect patient privacy and meet regulatory requirements such as HIPAA in the U.S. and GDPR in Europe.
- Authentication and Authorization: Protocols like OAuth 2.0 ensure that only authorized users and applications access health data, enforcing strict permissions and scopes.
- Encryption: Data is encrypted both in transit and at rest using industry-standard methods such as TLS/SSL to prevent unauthorized interception or tampering.
- Audit Logging: APIs keep detailed logs of all data access and transactions, enabling monitoring, compliance reporting, and forensic analysis if needed.
Strong security builds trust among patients, providers, and regulators, which is vital for broad API adoption.
Flexibility and Integration with Legacy Systems
Many healthcare providers operate legacy systems that were not designed with interoperability in mind. APIs provide a flexible integration layer that can connect these older systems with modern platforms.
For example, middleware solutions can wrap legacy EHRs and translate data into FHIR-compliant messages, enabling real-time data sharing without replacing costly core systems. This approach allows healthcare organizations to modernize gradually, minimizing disruption.
APIs also support multiple communication styles (REST, SOAP, GraphQL), allowing diverse applications—from mobile health apps to enterprise software—to connect smoothly.
Scalability: Meeting Growing Demands
As healthcare data volumes increase exponentially—driven by continuous monitoring devices, genomic data, and AI analytics—interoperability solutions must scale efficiently.
Cloud-native API management platforms provide features like auto-scaling, load balancing, and high availability to handle surges in traffic. During public health emergencies or mass vaccination campaigns, scalable APIs ensure that data flows uninterrupted to clinicians and public health officials.
Challenges and Considerations in Implementing Healthcare APIs
While healthcare APIs are key to unlocking interoperability, their implementation involves navigating a complex landscape of technical, organizational, and regulatory challenges.
1. Data Standardization and Semantic Interoperability
Even with widespread adoption of standards like FHIR, consistent interpretation and implementation remain challenging. Different systems might use varying terminologies or code systems, risking miscommunication. For example, a lab test result coded in one system may be interpreted differently by another, leading to potential clinical errors.
Achieving true semantic interoperability where data exchanged is both syntactically and meaningfully consistent requires ongoing collaboration among healthcare providers, vendors, and standards organizations. This includes agreeing shared vocabulary and mapping legacy codes to standardized formats.
2. Security and Privacy Concerns
Healthcare data is among the most sensitive to personal information, and APIs inherently increase the points of access, expanding potential vulnerabilities. A breach or unauthorized access could have severe consequences for patient privacy and trust.
Healthcare organizations must implement robust security frameworks incorporating:
- Multi-factor authentication
- End-to-end encryption
- Role-based access control
- Continuous monitoring and anomaly detection
High-profile cyberattacks targeting healthcare APIs have underscored the need for vigilance. Compliance with HIPAA, GDPR, and other regulations is not optional but fundamental.
3. Integration with Legacy Systems
Many healthcare systems run on legacy platforms that were never designed for modern interoperability. Retrofitting these systems with APIs often requires custom middleware or adapters, which can be costly and time-consuming.
Healthcare organizations must carefully balance the need for modernization with the risk of disrupting mission-critical workflows. Phased approaches that incrementally introduce API layers allow for smoother transitions and risk mitigation.
4. Regulatory and Compliance Complexity
Healthcare data exchange must comply with a patchwork of regulations varying by region and jurisdiction. Ensuring APIs enforce patient consent, data minimization, and auditability is complex but essential.
Data residency requirements, cross-border data flows, and patient access rights add layers of legal complexity that organizations must navigate carefully to avoid penalties and preserve patient trust.
5. Organizational Readiness and Cultural Barriers
Interoperability is not just a technical problem but a people and process challenge. Resistance to change, siloed departments, and lack of interoperability awareness can slow adoption.
Successful API projects require strong leadership support, clear governance policies, and ongoing training to align clinical and IT teams around shared interoperability goals.
6. Resource and Expertise Constraints
Designing, implementing, and maintaining secure and compliant APIs requires specialized expertise that many healthcare organizations lack internally. Hiring or partnering with experienced vendors is often necessary but can strain budgets.
Long-term success depends on investing in skills development and choosing scalable API management platforms that reduce operational complexity.
Examples of Healthcare APIs Driving Interoperability
Google Cloud Healthcare API
Google Cloud’s Healthcare API supports HL7v2, FHIR, and DICOM data standards, enabling healthcare organizations to ingest, store, and analyze clinical data securely in the cloud. Its integration with Google’s AI and machine learning tools empowers providers to gain insights from large datasets while maintaining strict compliance with privacy regulations.
Hospitals use this platform to modernize legacy data stores and enhance analytics capabilities, improving population health management and clinical decision support.
FHIR (Fast Healthcare Interoperability Resources)
FHIR’s open, web-friendly standard has become the backbone of modern healthcare APIs. Major EHR vendors such as Epic, Cerner, and Allscripts offer FHIR-compliant APIs, enabling developers to build interoperable applications that can access patient data across systems.
Apple Health Records exemplifies FHIR’s potential, allowing patients to aggregate health information from multiple providers securely on their iPhones, fostering patient-centered care.
MyHealthEData Initiative
This U.S. Department of Health and Human Services program promotes patient access and interoperability by encouraging the adoption of API standards like FHIR. It has accelerated the healthcare industry’s shift towards open data sharing, helping patients move their health records easily between providers and apps.
SMART on FHIR
SMART (Substitutable Medical Applications and Reusable Technologies) on FHIR is an open framework that enables third-party healthcare applications to integrate seamlessly with EHRs through standardized APIs. It allows providers and patients to use innovative digital tools for care management, clinical decision support, and analytics without vendor lock-in.
Conclusion
Healthcare APIs are the cornerstone of modern interoperability, transforming fragmented systems into interconnected networks that enhance care quality, patient engagement, and operational efficiency. While challenges in standardization, security, and integration persist, the strategic adoption of APIs rooted in robust standards and strong governance—unlocks tremendous potential.
By investing in scalable, secure API frameworks and fostering collaboration across clinical and IT teams, healthcare organizations can accelerate their journey toward a truly connected, patient-centered ecosystem. These interoperability solutions not only improve outcomes but also prepare healthcare systems to meet future demands in an increasingly data-driven world.
