The Clinician’s Guide to Modern Cardiac Monitoring
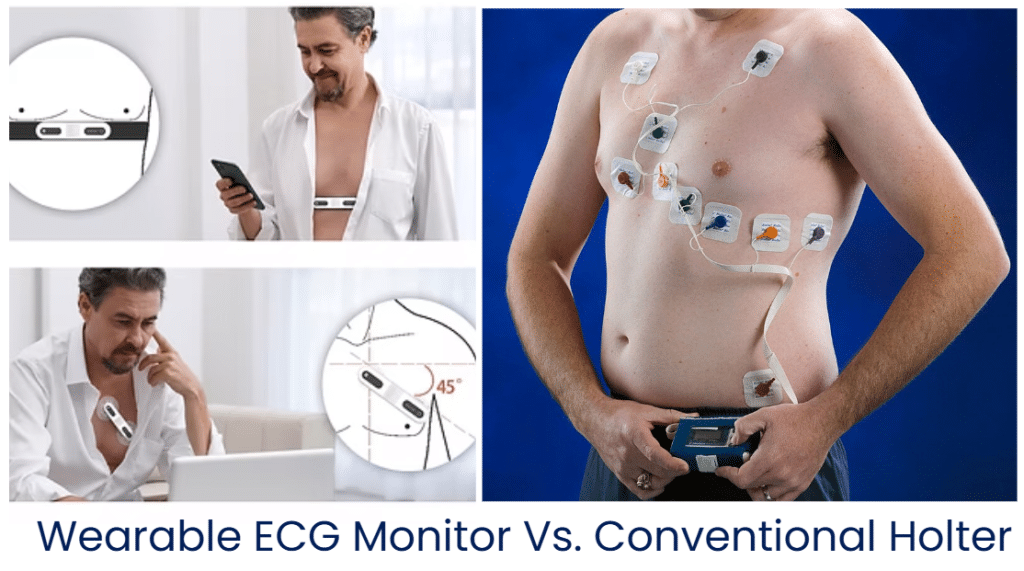
Balancing diagnostic accuracy in cardiac care with patient compliance and operational efficiency is quite a tough task for clinic managers and physicians. Two primary modalities dominate: the conventional Holter monitor and the digital-age wearable ECG monitoring device.
Historically, cardiac monitoring followed a snapshot model. If a patient’s symptoms didn’t occur during a 10-second resting ECG or a 24-hour Holter window, the diagnosis often remained elusive. This led to a high rate of undetected paroxysmal arrhythmias, such as Atrial Fibrillation (AFib).
The emergence of continuous wearable ECG monitoring has bridged this gap. Conventional Holter monitors are often perceived as short-term deep dives, while wearable monitors are designed for long-term vigilance. Wearable ECG monitors extend the window from days to weeks; now we can detect hidden arrhythmias that occur only once or twice a week.
But the question remains for many practitioners: can these sleek, user-friendly wearables truly replace the Holter system?
The answer is nuanced: While wearables are revolutionizing long-term screening and patient engagement, the Holter remains indispensable for specific morphology analyses.
Wearable ECG Monitor vs. Conventional Holter: A Head-to-Head Comparison
There are four aspects for clinics to evaluate whether an ECG monitor works efficiently: device profile, clinical effectiveness, workflow, and economic. Here we extend them to eight details:
1. Typical Use Duration
- Conventional Holter: Typically limited to 24 to 48 hours. Highly detailed, but this short window is a visible obstacle for paroxysmal events.
- Wearable ECG Monitor: Designed for extended use, often 72 hours. Research indicates that 7 to 8 days is the sweet spot for detecting paroxysmal AFib, capturing approximately 96% of arrhythmia events. [1]
2. Form & Specification Factors
- Conventional Holter: Usually about the size of a smartphone, connected to the patient via 5 to 7 lead wires and adhesive electrodes. The bulkiness requires the device to be worn on a belt or in a pocket.
- Wearable ECG Monitor: Wireless and lightweight. Some models in the market weigh only 13 grams and are just 0.8 cm thick. These devices utilize a single-lead patch or a chest strap, making them significantly less intrusive.
3. Patient Comfort and Compliance
If a patient removes a device due to irritation, the diagnostic value drops to zero.
- Holter: The wires can tangle, limit movement, and prevent showering, leading to a comfort rating of only about 51% in patient surveys.
- Wearables: Wireless patches allow for exercise, sleep, and daily activities without disruption. Studies show that 93% of patients find wearable patches comfortable, which translates directly to higher data completion rates.[1]

4. Diagnostic Yield and Accuracy
- Holter: Holter provides multi-lead data and is less likely to be affected by motion artifacts and electromagnetic interference.
- Wearables: Most wearable devices are single-lead (single-vector), which may cause them to miss certain complex waveform changes that are only apparent in specific spatial dimensions (such as complex morphological analysis or myocardial infarction). But medical-grade wearables are now showing a trend of rivaling traditional systems. A 72-hour wearable monitor has been shown to detect AFib at a rate 1.6 times higher than a 24-hour Holter. For paroxysmal AFib, the yield increases to 2.2 times. [2] Some medical-grade wearable ECG monitors boast a 90.2% classification accuracy, ensuring that the data you review is clinically actionable. [3]
5. Convenience of Data Review and Workflow
- Holter: This is a retrospective analysis model. The patient must return to the clinic, the data is downloaded, and a technician or physician manually interprets the entire 24–48 hour strip.
- Wearables: Many devices support real-time transmission via Bluetooth to a smartphone or cloud platform. AI-assisted reports can be available within minutes of the session’s end, allowing for faster clinical intervention.
6. Required Skills to Read and Interpret
Interpreting ECG data is a specialized skill that can often be a bottleneck in a busy clinic.
- Manual Interpretation: Traditional Holter reading requires a high level of expertise. 90% of physicians believe that data from patch monitors can yield definitive diagnoses, whereas only 64% hold this view regarding Holter monitors. [1]
- AI-Assisted Interpretation: Modern wearables leverage AI to perform preliminary screenings. This doesn’t replace the physician but acts as a powerful triage tool. To understand the intricacies of these waveforms, clinicians can refer to Viatom’s guide on how to read an ECG. Furthermore, the debate on whether AI can read ECG strips is evolving, with AI proving to be an essential partner in reducing physician burnout by highlighting only the most relevant anomalies.
7. Regulatory Status and Clinical Role
- Holter: Established clinical standard for decades. ESC and AHA have clear guides for their clinical usage.
- Wearables: Categorized into Medical-Grade (FDA-cleared for clinical decision-making) and Consumer-Grade (wellness-focused). For clinical practice, only medical-grade devices should be utilized to ensure the data stands up to diagnostic scrutiny.
8. Cost-Effectiveness and ROI
For clinic managers, the ROI of a wearable ECG monitor is found in the reduction of repeat testing. While the per-unit cost of a patch may be higher than a reusable Holter lead, the ability to reach a diagnosis in a single 7-day session—rather than three failed 24-hour sessions—results in significant long-term savings for the healthcare system and the patient.
Applicable Scenarios for the Two ECG Monitors
Neither device is a universal solution. The choice depends on the patient’s specific clinical presentation.
The Wearable ECG Monitor is best for:
- Capture of Infrequent Symptoms: Patients reporting palpitations or dizziness that occur only once or twice a week.
- High-Activity Patients: Those who need to maintain an active lifestyle, exercise, or travel during the monitoring period.
- Remote Patient Monitoring (RPM): Ideal for post-discharge monitoring of elderly patients or those in rural areas who cannot easily return to the clinic for data downloads.
The Conventional Holter Monitor is best for:
- Complex Morphology Analysis: When a physician needs multi-lead (3, 5, or 12-lead) data to analyze specific P-wave or QRS complex morphology.
- Frequent Daily Symptoms: If a patient is experiencing symptoms multiple times a day, a 24-hour high-fidelity window is often sufficient and highly efficient.
- Surgical Pre-Assessment: When a comprehensive snapshot is required within a strictly defined 48-hour window.
The Next Steps for Wearable ECG Monitor & Conventional Holter Monitor? Will They Coexist?
The future of cardiac monitoring is not a winner-takes-all scenario. Instead, we are moving toward a Layered Care Model.
In this model, the wearable ECG monitoring device sits on the front lines, monitoring patients in their natural environments, using AI to sift through weeks of data to find the needle in the haystack. Once an abnormality is flagged, the conventional Holter or a 12-lead ECG acts as the specialist, providing the high-resolution detail needed for surgical planning or complex pathological diagnosis.
By 2028, the global wearable medical device market is projected to reach $70 billion. For American clinics, integrating these technologies means moving from a reactive wait-and-see approach to a proactive detect-and-protect strategy. [4]
About Viatom
Viatom is a global leader in innovative medical electronics, specializing in wearable and handheld ECG technology. Their mission is to provide clinicians with the tools they need to make faster, more accurate diagnoses while improving the patient experience. Explore their range of ECG monitors today.
*Disclaimer: The information provided in this article is for educational and informational purposes only and is not intended as medical advice. Always seek the advice of a qualified healthcare provider with any questions regarding a medical condition or the interpretation of ECG data.