Rheumatoid arthritis (RA) is a long-term autoimmune disease that causes pain, stiffness, and swelling in different types of joints throughout the body, impacting millions of people in the world and often breaking up their daily activities. Even after taking conventional treatments, like NSAIDs and DMARDs, some people do not achieve adequate relief. In such cases, infusion therapy can be a significant option for RA patients. This treatment involves administering medication directly into the patient’s bloodstream through an IV, targeting specific parts of the immune system to help reduce inflammation. After receiving this therapy, patients reported less pain and improved their joint function. However, it is essential to consult your Doctor before starting this treatment.
Understanding Infusion Therapy
Infusion therapy is a treatment method in that medication is directly administered into the bloodstream through an IV. This approach allows the medication to work more quickly and effectively in the body than oral medicine. IV infusion is particularly beneficial for rheumatoid arthritis patients, especially those suffering from moderate to severe stages. Additionally, it is helpful for those who cannot tolerate the side effects of oral medications. For patients who do not achieve appropriate results from traditional treatments, infusion therapy can be a viable option.
Benefits of Infusion Therapy
- Rapid Action: Infusions can provide faster relief than oral medications, within few hours or days.
- Higher Drug Concentration: Since it is administered directly into the bloodstream, and more effective dosages can be provided.
- Targeted Treatment: Infusion therapy can provide more advanced treatment by targeting specific pathways involved in rheumatoid arthritis.
- Convenience: Infusions are usually treated in a clinical setting.
How Infusion Therapy Works
Infusion therapy for rheumatoid arthritis mainly uses medications made from living organisms that target inflammation in the body. These treatments focus on specific parts of the immune system, it is helped to reduce swelling, relieve pain, and protect the joints from damage.
Types of Infusions for Rheumatoid Arthritis
There are several types of infusion therapies for rheumatoid arthritis, and each one works in its way and has different treatment plans:
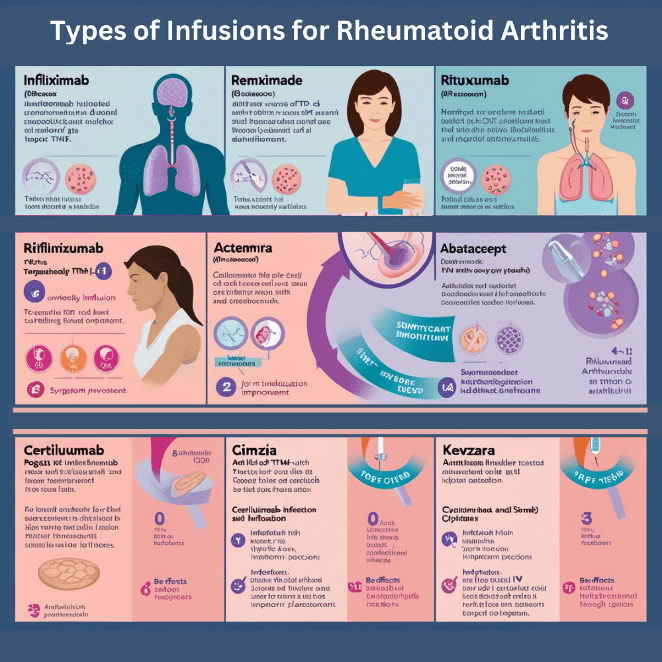
1. Infliximab (Remicade)
- Mechanism: Infliximab is a medicine that stops the action of a protein called TNF, which causes inflammation in the body.
- Administration: You start with three infusions at weeks 0, 2, and 6, and then continue with one infusion every 8 weeks.
- Benefits: It is effective in reducing rheumatoid arthritis symptoms, helping with physical abilities, and slowing down the progress of the disease.
- Potential Side Effects: There is a risk of infections, reactions during the infusion (like fever and chills), and the possibility of the body making antibodies against the medicine.
2. Rituximab (Rituxan)
- Mechanism: Rituximab is a type of medicine that targets B cells with a protein called CD20, which is involved in the inflammation process of rheumatoid arthritis.
- Administration: You get two infusions two weeks apart, and then you usually have maintenance infusions every 6 months.
- Benefits: It can greatly improve symptoms in patients who don’t respond to other treatments and is considered safe to use.
- Potential Side Effects: Possible side effects include infusion reactions like headaches and fever, a higher chance of infections, and the risk of serious allergic reactions.
3. Tocilizumab (Actemra)
- Mechanism: Tocilizumab is a medicine that blocks IL-6, a protein involved in inflammation, helping to reduce swelling in rheumatoid arthritis.
- Administration: It is given as an IV infusion every 4 weeks.
- Benefits: It is effective in reducing symptoms of rheumatoid arthritis, and it also improves quality of life while preventing joint damage.
- Potential Side Effects: Possible side effects include elevated liver enzymes, a higher risk of infections, and gastrointestinal perforations.
4. Abatacept (Orencia)
- Mechanism: Abatacept stops T-cell activation, which is an important part of the immune response that causes joint inflammation.
- Administration: It is given as an initial infusion, followed by doses at 2 weeks and 4 weeks, and then every 4 weeks after that.
- Benefits: It can be used with other DMARDs and has a lower risk of serious infections compared to other biological medications.
- Potential Side Effects: Headaches, infections, and reactions related to the infusion.
5. Golimumab (Simponi Aria)
- Mechanism: It is another TNF-alpha inhibitor that reduces inflammation by stopping the action of TNF.
- Administration: It is given as an infusion at the start and then every 8 weeks.
- Benefits: It offers significant relief from symptoms and improves physical function, with an easy dosing schedule.
- Potential Side Effects: Like other TNF inhibitors, it carries risks of infections and infusion reactions.
6. Certolizumab Pegol (Cimzia)
- Mechanism: It is a pegylated Fab’ fragment of a humanized anti-TNF antibody that attaches to TNF and stops it from activating its receptor.
- Administration: It is administered as a subcutaneous injection at weeks 0, 2, and 4, after which it is given every 4 weeks to maintain its therapeutic effects.
- Benefits: It helps reduce the signs and symptoms of rheumatoid arthritis while also improving physical function.
- Potential Side Effects: Possible side effects include injection site reactions, headaches, and a higher risk of infections.
7. Sarilumab (Kevzara)
- Mechanism: This is another IL-6 receptor antagonist that helps lower inflammation in patients with rheumatoid arthritis.
- Administration: It is administered as an injection under the skin once every two weeks.
- Benefits: It helps reduce symptoms and improve physical function, especially for patients who haven’t improved with other treatments.
- Potential Side Effects: There is a risk of infections, increased liver enzymes, and reactions at the injection site.
Tofacent and Baricinix: Innovations in RA Infusion Therapy
Newer medicines like Tofacitinib 5 mg and Baricitinib 4 mg are new choices for treating rheumatoid arthritis. These medicines, which belong to a class known as Janus kinase (JAK) inhibitors, are employed to treat various inflammatory conditions due to their ability to modulate the immune response. They work by targeting the JAK-STAT signaling pathway, which is important for the immune response and inflammation.
Tofacent 5 mg
Tofacent (tofacitinib) is a JAK inhibitor that has been very effective in reducing symptoms of rheumatoid arthritis and improving physical function. It operates through the inhibition of Janus kinase enzymes, which are crucially implicated in the inflammatory processes associated with rheumatoid arthritis. Tofacent can be taken by mouth or given as an infusion, and the infusion option can provide faster relief for severe symptoms.
Learn more about Tofacent 5 mg treatment
Baricinix 4 mg
Baricinix (baricitinib) is another JAK inhibitor that targets the JAK1 and JAK2 enzymes. Clinical studies have shown that it effectively reduces joint pain, swelling, and overall disease activity in patients with rheumatoid arthritis. Baricinix is especially helpful for patients who do not get enough relief from TNF inhibitors. Like Tofacent, Baricinix can be taken by mouth or given as an infusion, making it a flexible choice for managing rheumatoid arthritis.
Learn more about Baricinix 4 mg treatment
What to Expect During Infusion Treatment
Rheumatoid arthritis infusion therapy involves several steps:
1. Pre-Infusion Assessment
Prior to initiating the infusion, healthcare providers will conduct a comprehensive assessment to evaluate the patient’s condition and determine the most appropriate treatment approach. This may include:
- A detailed medical history, including current medications and any previous treatments for RA.
- Blood tests are performed to check how well the liver and kidneys are working and to check for any infections.
- Discussing potential side effects is important, and it is also essential to explore effective strategies for managing these reactions.
2. Infusion Process
The infusion itself can take between 30 minutes to a few hours, depending on the medication and dose. Patients are usually watched for any immediate reactions during this time. The steps typically include:
- Setting Up: A healthcare worker will put an IV catheter into a vein, usually in the arm.
- Infusion: The medication is given through the IV, and the patient is watched for any bad reactions.
- Comfort Measures: Patients may receive blankets, snacks, or drinks to make them feel more comfortable during the infusion.
3. Post-Infusion Care
After the infusion, patients may be watched briefly to check for any bad reactions. Common side effects can include:
- Mild Headaches: These can happen after the infusion but usually go away within a few days.
- Fatigue: Some patients may feel tired after treatment, and others might experience different side effects as well.
- Nausea: A rare but possible side effect.
4. Ongoing Monitoring
Regular follow-up appointments are important to check how well the treatment is working. Healthcare providers will:
- Check how the patient responds to the medication and change the treatment if needed.
- Watch for possible side effects, including infections or problems with organ function.
5. Lifestyle Considerations
Patients receiving infusion therapy for RA are encouraged to:
- Keep a healthy lifestyle by eating a balanced diet and exercising regularly to help manage symptoms and improve overall health.
- Patients should remain informed about their condition and treatment options to make educated decisions regarding their healthcare.
- Talk openly with healthcare providers about any worries or side effects.
Conclusion
Infusion therapy can be a useful treatment for rheumatoid arthritis, especially for people who do not get good results from regular therapies. With different options available, patients should talk to a healthcare provider about their specific needs to find the best plan of action. Knowing about infusions for rheumatoid arthritis helps patients make informed choices about their treatment and improves their quality of life.
If you or someone you care about is thinking about infusion therapy for RA, talk to a rheumatologist to explore options and create a personalized treatment plan. Managing rheumatoid arthritis can be tough, but with the right treatments and support, patients can find relief and live satisfying lives.
