Contaminated medical gases are an invisible threat in healthcare settings. Oxygen, nitrous oxide, and medical air play vital roles in surgical procedures, intensive care, and respiratory therapy. But if these gases contain even small amounts of oil, bacteria, or moisture, the effects can be devastating—equipment failure, compromised anesthesia delivery, and increased infection rates. The problem is that contamination often goes unnoticed until it causes serious harm.
Regulatory bodies like NFPA 99, OSHA, and the FDA have established strict gas purity standards, but compliance is not always enough. Contamination can still occur due to poor medical gas installation, neglected maintenance, or aging pipelines. Recognizing the risks and implementing proactive prevention strategies is essential for ensuring safe and effective medical treatment.
How Gas Contamination Affects Medical Procedures
Contaminated medical gases can cause complications ranging from minor system inefficiencies to life-threatening patient outcomes. The presence of particulates, moisture, oil, or microbial growth in a gas supply can severely impact hospital operations.
Sources of Contamination in Medical Gas Systems
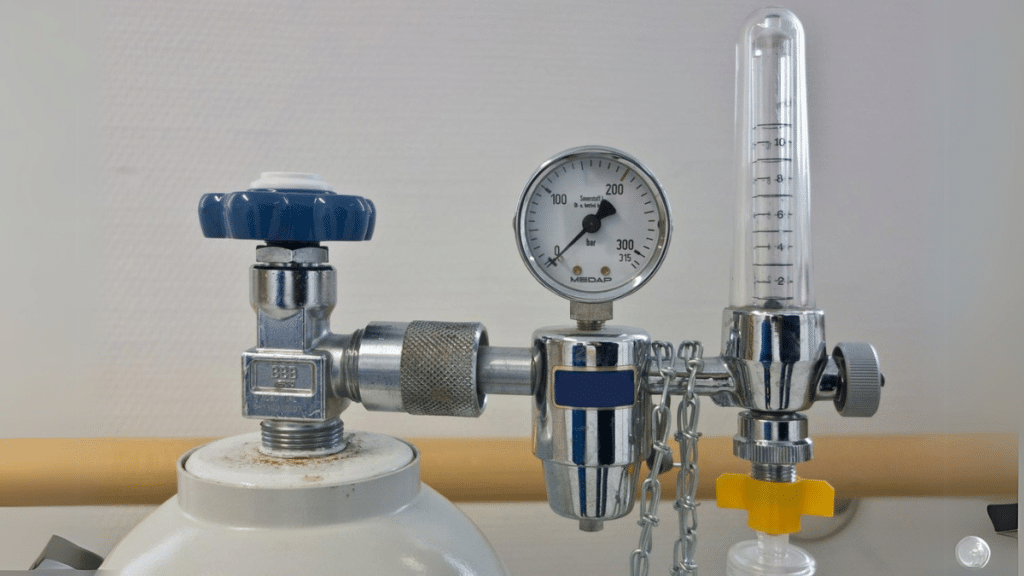
Medical gas systems are designed to deliver high-purity gases, but contamination can still occur at multiple points:
- Poor medical gas installation – If the pipeline is not properly cleaned before installation, residual oil, dust, and debris can enter the system. Even small amounts of contaminants can lead to oxygen ignition risks or equipment malfunctions.
- Cross-contamination – Leaking valves or incorrect piping layouts can cause unintended gas mixing. For example, nitrogen entering an oxygen supply could lead to hypoxic conditions.
- Moisture buildup – Excess moisture in medical air lines can encourage bacterial growth, potentially leading to infections when used in patient ventilators or anesthesia machines.
- Aging infrastructure – Over time, medical gas pipes can develop corrosion, leading to particulate contamination that damages equipment and compromises gas purity.
Consequences of Contaminated Medical Gases
Gas contamination is more than a minor inconvenience—it directly affects patient safety and the efficiency of medical procedures.
- Patient Health Risks – A 2018 study by the World Health Organization found that unclean medical gases contributed to post-surgical infections in 8% of cases where contamination was detected. Oxygen lines with bacterial growth pose a direct risk to immunocompromised patients.
- Anesthesia Complications – Even a small deviation in gas composition can lead to incorrect dosages during surgeries. This increases the risk of adverse reactions or prolonged recovery times.
- Equipment Damage – Medical gas-powered devices, including ventilators and anesthesia machines, rely on pure gases to function correctly. Contaminants can clog internal components, leading to costly repairs or system failures at critical moments.
- Regulatory Violations – The Joint Commission and NFPA 99 require strict adherence to gas purity standards. Facilities that fail routine inspections due to contaminated gases can face fines, accreditation loss, or forced system shutdowns.
Preventing Gas Contamination in Healthcare Facilities
Preventing contamination requires a combination of proper system installation, routine monitoring, and timely upgrades.
Proper Medical Gas Installation & Maintenance
One of the most effective ways to reduce contamination risks is ensuring medical gas installation is done correctly from the start. Certified medical gas installers follow strict cleaning procedures to remove residual oil and debris before sealing the system.
Facilities should also:
- Use ASSE 6010-certified medical gas installers for all installations and modifications.
- Implement a leak detection program to identify and repair any potential gas leaks.
- Perform regular purging and system flushing to remove built-up contaminants.
Routine Monitoring and Testing for Gas Purity
Even a properly installed system can develop contamination issues over time. Routine gas purity testing helps facilities stay ahead of potential problems.
- Gas sampling and analysis should be conducted quarterly to detect microbial growth, oil particulates, and moisture levels.
- Medical gas alarms should be installed at key points to detect pressure drops or gas composition changes in real time.
- NFPA 99-mandated inspections should be followed to ensure compliance with purity standards.
Upgrading Outdated or Poorly Installed Systems
Older hospitals and clinics often rely on aging pipelines that do not meet modern purity standards. In these cases, replacing outdated equipment and pipes is the only solution to maintain compliance and patient safety.
- Facilities should evaluate systems older than 20 years for potential contamination risks.
- Certified medical gas installers should be consulted before making any modifications to ensure compliance with current NFPA 99 standards.
- Newer pipeline materials and automated monitoring systems should be considered to improve long-term reliability.
Conclusion
Gas contamination in medical facilities is a serious risk that can impact patient outcomes, equipment functionality, and regulatory compliance. While the contamination can stem from poor medical gas installation, aging infrastructure, or system failures, the good news is that preventive maintenance, routine gas purity testing, and working with qualified medical gas installers can significantly reduce these risks.
Hospitals and healthcare facilities must prioritize gas purity as part of their overall safety and compliance strategy. Contaminated medical gases are not just a technical issue—they are a direct threat to patient care. Addressing these risks now ensures a safer environment for both patients and medical staff.